
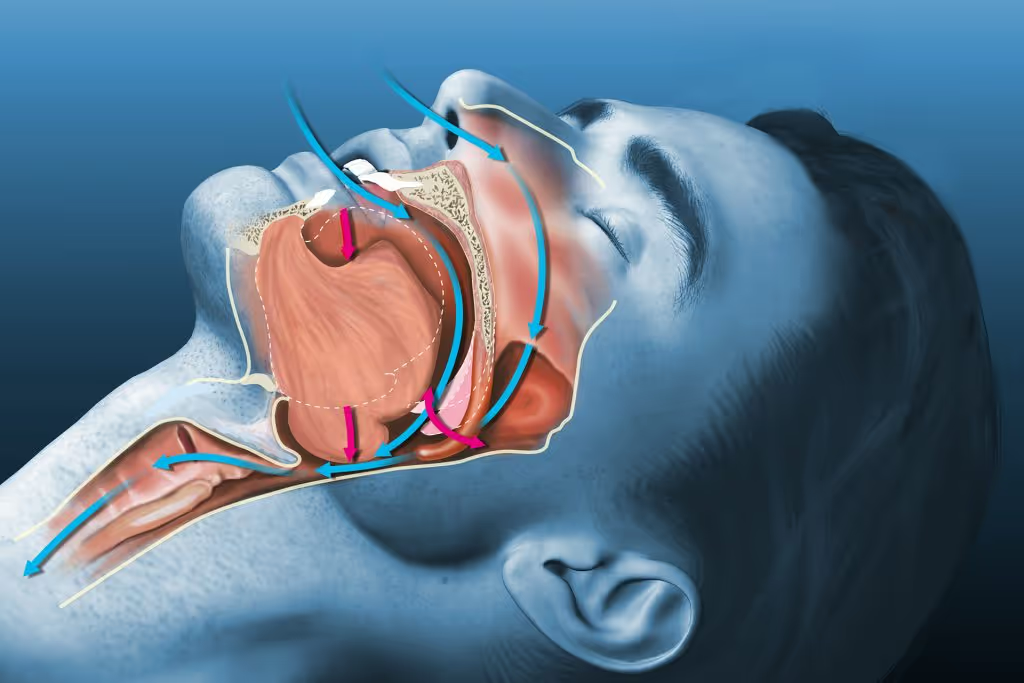
Normally during sleep, air moves through the throat and in and out of the lungs at a regular rhythm. In a person with sleep apnea, air movement is periodically diminished or stopped. There are two types of sleep apnea: obstructive sleep apnea and central sleep apnea.
In obstructive sleep apnea, breathing is abnormal because of narrowing or closure of the throat. In central sleep apnea, breathing is abnormal because of a change in the breathing control and rhythm.
Sleep apnea is a serious condition that can affect a person’s ability to safely perform normal daily activities and can affect long term health. Approximately 25 percent of adults are at risk for sleep apnea of some degree. Men are more commonly affected than women. Other risk factors include middle and older age, being overweight or obese, and having a small mouth and throat. The most common type of sleep apnea in adults is obstructive sleep apnea (OSA).
The throat is surrounded by muscles that control the airway for speaking, swallowing, and breathing. During sleep, these muscles are less active, and this causes the throat to narrow. In most people, this narrowing does not affect breathing. In others, it can cause snoring, sometimes with reduced or completely blocked airflow.
A completely blocked airway without airflow is called an obstructive apnea. Partial obstruction with diminished airflow is called a hypopnea. A person may have apnea and hypopnea during sleep. Insufficient breathing due to apnea or hypopnea causes oxygen levels to fall and carbon dioxide to rise. Because the airway is blocked, breathing faster or harder does not help to improve oxygen levels until the airway is reopened.
Typically, the obstruction requires the person to awaken to activate the upper airway muscles. Once the airway is opened, the person then takes several deep breaths to catch up on breathing.
As the person awakens, he or she may move briefly, snort or snore, and take a deep breath. Less frequently, a person may awaken completely with a sensation of gasping, smothering, or choking.
If the person falls back to sleep quickly, he or she will not remember the event. Many people with sleep apnea are unaware of their abnormal breathing in sleep, and all patients underestimate how often their sleep is interrupted. Awakening from sleep causes sleep to be unrefreshing and causes fatigue and daytime sleepiness.
Most patients have OSA because of a small upper airway. As the bones of the face and skull develop, some people develop a small lower face, a small mouth, and a tongue that seems too large for the mouth. These features are genetically determined, which explains why OSA tends to cluster in families. Obesity is another major factor. Tonsil enlargement can be an important cause, especially in children.
The main symptoms of OSA are loud snoring, fatigue, and daytime sleepiness. However, some people have no symptoms. For example, if the person does not have a bed partner, he or she may not be aware of the snoring. Fatigue and sleepiness have many causes and are often attributed to overwork and increasing age. As a result, a person may be slow to recognize that they have a problem. A bed partner or spouse often prompts the patient to seek medical care.
Other symptoms may include one or more of the following:
Complications of sleep apnea can include daytime sleepiness and difficulty concentrating. The consequence of this is an increased risk of accidents and errors in daily activities. Studies have shown that people with severe OSA are more than twice as likely to be involved in a motor vehicle accident as people without these conditions. People with OSA are encouraged to discuss options for driving, working, and performing other high-risk tasks with a healthcare provider.
In addition, people with untreated OSA may have an increased risk of cardiovascular problems such as high blood pressure, heart attack, abnormal heart rhythms, or stroke. This risk may be due to changes in the heart rate and blood pressure that occur during sleep.
The diagnosis of OSA is best made by a knowledgeable sleep medicine specialist who has an understanding of the individual’s health issues. The diagnosis is usually based upon the person’s medical history, physical examination, and testing, including:
Testing is usually performed in a sleep laboratory. A full sleep study is called a polysomnogram. The polysomnogram measures the breathing effort and airflow, blood oxygen level, heart rate and rhythm, duration of the various stages of sleep, body position, and movement of the arms/legs.
Home monitoring devices are available that can perform a sleep study. This is a reasonable alternative to conventional testing in a sleep laboratory if the clinician strongly suspects moderate or severe sleep apnea and the patient does not have other illnesses or sleep disorders that may interfere with the results.
Sleep apnea is best treated by a knowledgeable sleep medicine specialist. The goal of treatment is to maintain an open airway during sleep. Effective treatment will eliminate the symptoms of sleep disturbance; long-term health consequences are also reduced. Most treatments require nightly use. The challenge for the clinician and the patient is to select an effective therapy that is appropriate for the patient’s problem and that is acceptable for long term use.
The most effective treatment for sleep apnea uses air pressure from a mechanical device to keep the upper airway open during sleep. A CPAP device uses an air-tight attachment to the nose, typically a mask, connected to a tube and a blower which generates the pressure. Devices that fit comfortably into the nasal opening, rather than over the nose, are also available. CPAP should be used any time the person sleeps (day or night).
The CPAP device is usually used for the first time in the sleep lab, where a technician can adjust the pressure and select the best equipment to keep the airway open. Alternatively, an “auto” device with a self-adjusting pressure feature, provided with proper education and training, can get treatment started without another sleep test. While the treatment may seem uncomfortable, noisy, or bulky at first, most people accept the treatment after experiencing better sleep. However, difficulty with mask comfort and nasal congestion prevent up to 50 percent of people from using the treatment on a regular basis.
Continued follow up with a healthcare provider helps to ensure that the treatment is effective and comfortable.
Information from the CPAP machine is often used by physicians, therapists, and insurers to track the success of treatment. CPAP can be delivered with different features to improve comfort and solve problems that may come up during treatment. Changes in treatment may be needed if symptoms do not improve or if the person’s condition changes, such as a gain or loss of weight.
Adjusting sleep position (to stay off the back) may help improve sleep quality in people who have OSA when sleeping on the back. However, this is difficult to maintain throughout the night and is rarely an adequate solution.
Weight loss may be helpful for obese or overweight patients. Weight loss may be accomplished with dietary changes, exercise, and/or surgical treatment. However, it can be difficult to maintain weight loss; the five-year success of non-surgical weight loss is only 5 percent, meaning that 95 percent of people regain lost weight.
Alcohol can worsen sleepiness, potentially increasing the risk of accidents or injury. People with OSA are often counseled to drink little to no alcohol, even during the daytime. Similarly, people who take anti-anxiety medications or sedatives to sleep should speak with their healthcare provider about the safety of these medications.
People with OSA must notify all healthcare providers, including surgeons, about their condition and the potential risks of being sedated. People with OSA who are given anesthesia and/or pain medications require special management and close monitoring to reduce the risk of a blocked airway.
A dental device, called an oral appliance or mandibular advancement device, can reposition the jaw (mandible), bringing the tongue and soft palate forward as well. This may relieve obstruction in some people.
This treatment is excellent for reducing snoring, although the effect on OSA is sometimes more limited. As a result, dental devices are best used for mild cases of OSA, when relief of snoring is the main goal. Failure to tolerate and accept CPAP is another indication for dental devices. While dental devices are not as effective as CPAP for OSA, some patients prefer a dental device to CPAP. Side effects of dental devices are generally minor, but may include changes to the bite with prolonged use.
Surgery is an alternative therapy for patients who cannot tolerate or do not improve with nonsurgical treatments such as CPAP or oral devices. Surgery can also be used in combination with other nonsurgical treatments.
Surgical procedures reshape structures in the upper airways or surgically reposition bone or soft tissue.
Uvulopalatopharyngoplasty (UPPP) removes the uvula and excessive tissue in the throat, including the tonsils, if present. Other procedures, such as maxillomandibular advancement (MMA), address both the upper and lower pharyngeal airway more globally.
UPPP alone has limited success rates (less than 50 percent) and people can relapse (when OSA symptoms return after surgery). As a result, this surgery is only recommended in a minority of people and should be considered with caution. MMA may have a higher success rate, particularly in people with abnormal jaw (maxilla and mandible) anatomy, but it is the most complicated procedure. A newer surgical approach, nerve stimulation to protrude the tongue, has promising success rates in very selected people.
Tracheostomy creates a permanent opening in the neck. It is reserved for people with severe disease in whom less drastic measures have failed or are inappropriate. Although, it is always successful in eliminating obstructive sleep apnea, tracheostomy requires significant lifestyle changes and carries some serious risks (e.g., infection, bleeding, blockage).
All surgical treatments require discussions about the goals of treatment, the expected outcomes, and potential complications.